Search for Articles
Article Architecture Biology Engineering in General General Medicine Life Sciences and Basic Medicine Social Medicine
Accuracy of peripheral oxygen saturation (SpO₂) at rest determined by a smart ring: A Study in Controlled Hypoxic Environments
Journal Of Digital Life.2025, 5,6;
Received:June 15, 2025 Revised:July 17, 2025 Accepted:October 22, 2025 Published:December 4, 2025
- Hirotsugu Morinaga
- National Institute of Fitness and Sports in KANOYA
- Sabrina Crepaldi
- SOXAI Inc.
- Jiabin Wang
- SOXAI Inc.
- Naoki Otsuka
- National Institute of Fitness and Sports in KANOYA
- Tatsuhiko Watanabe
- SOXAI Inc.
- Yohei Takai
- National Institute of Fitness and Sports in KANOYA
Correspondence: y-takai@nifs-k.ac.jp
Abstract
Peripheral oxygen saturation (SpO₂) measured by small wearable devices has garnered significant attention as a tool for detecting vital signs in acute and chronic diseases. However, the accuracy of such devices, particularly smart rings measuring SpO₂ at the finger base, remains underexplored. This study aimed to validate the accuracy of SpO₂ measurements obtained from a smart ring by comparing them with a clinical pulse oximeter in a controlled hypoxic environment. A total of 10 active males and females lay in the supine position at rest in a hypoxic environment, where oxygen saturation was maintained between 80% and 100% (normoxic levels). The participants wore a smart ring with photoplethysmography at the base of the second and third fingers of the dominant hand and a clinical pulse oximeter on their fingertips. To validate the accuracy of SpO₂ measured by a smart ring, leave-one-out cross-validation was performed, comparing root-mean-square error (RMSE) for 6793 data samples. The mean SpO₂ was 88.3 ± 7.2% for the smart ring and 88.3 ± 8.0% for the clinical-grade pulse oximeter, with a RMSE of 3.55%. These findings suggest that the smart ring provides reasonably accurate SpO₂ readings at rest, supporting its potential utility for health monitoring.
1. Introduction
Vital signs such as blood pressure, heart rate, and peripheral oxygen saturation (SpO2) are essential for the early detection and diagnosis of various health conditions and illnesses (Singhal et al., 2023). In cases of respiratory and cardiovascular diseases, disruptions in pulmonary oxygen exchange and decreased oxygen transport to tissues result in lower SpO2 levels (Singhal et al., 2023). Hence, SpO2 is one of the vital signs specifically used as a critical diagnostic marker in diseases affecting the respiratory and circulatory systems, such as COVID-19 (Vogel et al., 2020).
SpO2 can be measured using a pulse oximeter that utilizes photoplethysmography (PPG) (ANALOG DEVICES, 2019). In recent years, PPG technology has been integrated into wearable devices, enabling continuous and effortless SpO2 monitoring. However, not only is research on the accuracy of SpO2 measurement using wearable devices limited, but their accuracy also remains inferior to that of clinical-grade pulse oximeters (Pracht, 2022). Research on the validity of SpO2 measurement with wearable devices in a prior study reported a root mean square error (RMSE) of 4.46% (Pracht, 2022), which is greater than the standard recommended by the Food and Drug Administration (FDA: <3.5%) and the International Organization for Standardization (ISO) 80601-2-61 (<4.0%).
To accurately calibrate an SpO2 estimation model, reference data should be collected across multiple oxygen saturation levels, incrementally increasing while maintaining a steady state at each level (ANALOG DEVICES, 2019). While methods like exercise and breathing control can be used to lower SpO2 levels, they are limited by their ability to maintain a steady state or achieve precise target levels. Alternatively, as blood oxygen levels are known to decrease in hypoxic environments (Otani et al., 2023), an environmental simulator can be used to precisely control inspired oxygen concentration in a stepwise manner.
Despite the growing popularity of wearable devices for health monitoring, the accuracy of SpO2 measurements obtained from smart rings remains poorly investigated. Although certain models incorporate parabolic reflectors and strategic sensor placement (Lu et al., 2015), they typically lack optical components that are essential for minimizing stray light and enhancing light collection efficiency (Hénault et al., 2013). To address these limitations, the smart ring employed in this study uses multiple-wavelength high-emitting diodes (LEDs) alongside multiple photodetectors to enable more accurate PPG signal acquisition. Therefore, the purpose of this study was to validate an SpO2 estimation model using this smart ring equipped with the specified optical elements, under controlled hypoxic conditions with an environmental simulator.
2. Methods
2.1. Participants
The study included 10 healthy adult participants with an athletic background, consisting of five males (22.2 ± 0.4 years,180.0 ± 6.1 cm,73.7 ± 6.7 kg) and five females (24.4 ± 5.9 years, 155.8 ± 2.5 cm, 54.7 ± 8.6 kg). All participants had more than five years of experience in competitive sports. Their athletic disciplines included soccer (n = 4), kendo (n = 2), middle-distance running (n = 2), windsurfing (n = 1), and canoeing (n = 1). To minimize potential confounding effects on SpO2 measurements, individuals with finger injuries were excluded. Due to the demographic composition of the local participant pool, individuals with darker skin pigmentation were not included in the study.
The study protocol was approved by the Ethics Committee of the National Institute of Fitness and Sports in Kanoya. All participants were fully informed about the study’s objectives and procedures, and written informed consent was obtained prior to participation.
2.2. Overview
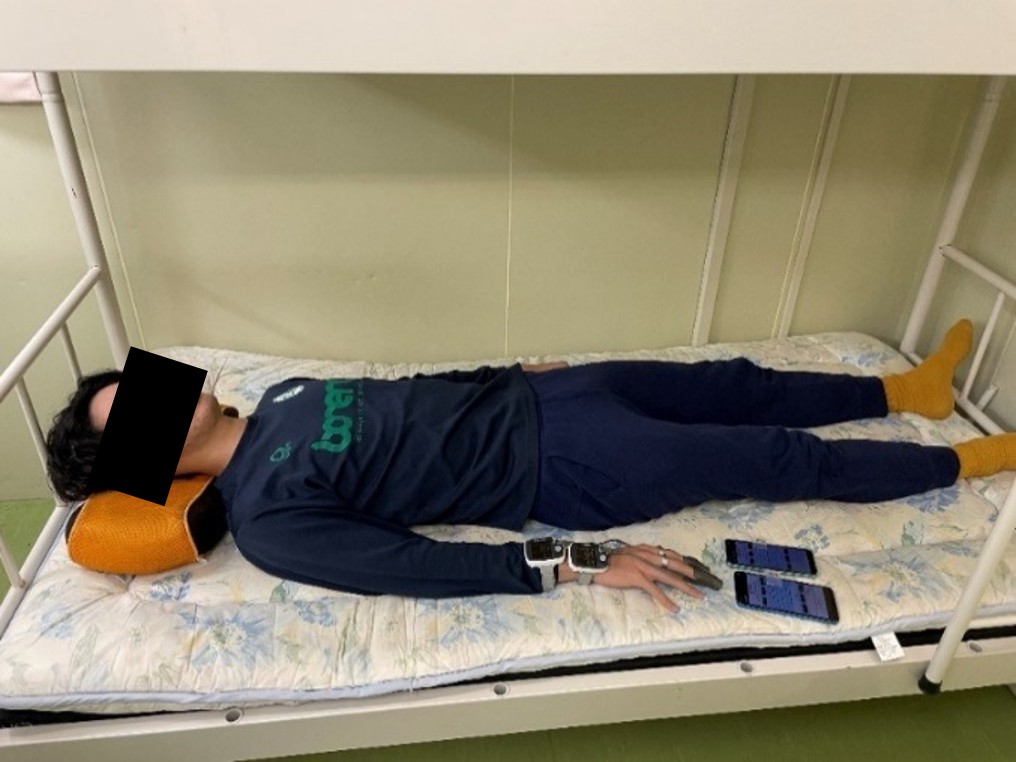
To minimize the influence of circadian variations, each participant completed two experimental sessions scheduled at the same time each day. For safety and consistency, participants remained in a supine position throughout the protocol in a controlled environment, which included both a normobaric normoxic laboratory setting (SpO2 range: 80%–100%) and a normobaric hypoxic environment simulated using an environmental chamber. The experimental conditions included five SpO2 levels: 100%, 95%, 90%, 85%, and 80%. The corresponding oxygen concentrations in the environment simulator were set to 20.6%, 16.0%, 14.5%, 13.1%, and 11.8%, respectively, based on preliminary experiments conducted prior to the main study. Upon their arrival at the laboratory, participants were first instructed to rest in a supine position in a normobaric normoxic environment. Subsequently, they were transferred to a normobaric hypoxic environment where they remained in the supine position. The hypoxic conditions were tested in two sequences: one with SpO2 levels ranging from 80 % to 90 % and another with levels ranging from 85 % to 95 %. These conditions were randomly assigned to participants on different days. Reference SpO2 was measured using a clinical-grade pulse oximeter placed on the second and third finger of the dominant hand. Simultaneously, PPG signals were recorded via a smart ring worn on the second and third finger of the same hand. After sufficient acclimatization and stabilization of SpO2 levels, data were collected for 30 to 120 seconds (Fig. 1).
2.3 Peripheral oxygen saturation (SpO2) measurement
SpO2 was measured using a smart ring (SOXAI Ring 1, SOXAI Inc., Japan) and a clinical-grade pulse oximeter (PULSOX-Me 500, TEIJIN, Japan). Measurements were taken on the second and third fingers of the dominant hand using both devices. Before taking measurements, participants were fitted with an appropriately sized smart ring, with its position adjusted to ensure proper data acquisition. Participants then assumed a supine position for the duration of the measurements. The clinical-grade pulse oximeter recorded data continuously throughout the entire experiment. Meanwhile, the smart ring measured the PPG signals in intervals ranging from 30 to 120 seconds, with each measurement manually triggered to align with the clinical-grade pulse oximeter. The smart ring measured two-channel PPG signals, with light sources of red (655 nm) and infrared (940 nm), respectively. The sampling rates of the PPG signals were both 100 Hz. The measured signals were sent in real-time to a smartphone through Bluetooth Low Energy communication. The smartphone saved the recorded data to its storage every 30 seconds. Measurements shorter than 30 seconds were discarded. SpO2 estimation and validation with the clinical-grade pulse oximeter was done offline. The clinical-grade pulse oximeter had a sampling frequency of 1 Hz, and the data output consisted of a 3-second moving average (Fig. 2). To synchronize the data sampling from both devices, the smart ring data were averaged over 1-second intervals. During the analysis, the start times of the smart ring and clinical-grade pulse oximeter were manually aligned and further fine-tuned using phase matching.
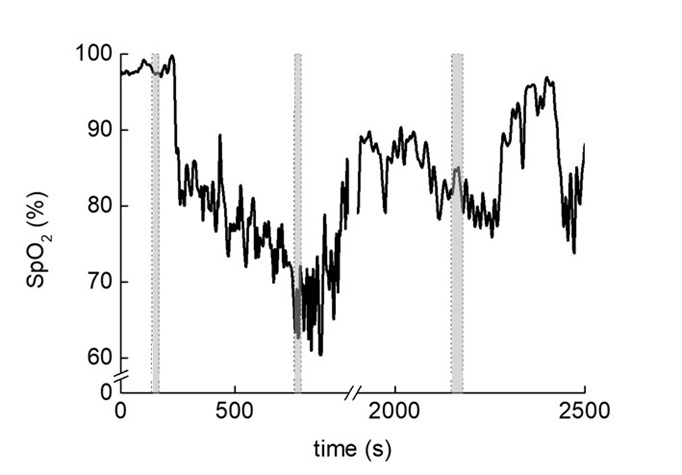
The black line represents SpO2 measured using a medical-grade pulse oximeter. The gray-shaded area indicates the time windows during which SpO2 measurements were acquired using the smart ring developed by SOXAI Inc.
2.4. Statistical analysis
The sample size calculation was based on the accuracy of testing guidelines for pulse oximeters in accordance with the International Organization for Standardization (ISO), which requires at least 200 data points from a minimum of 10 subjects, with a balanced range of arterial oxygen saturation from 70 % to 100 %. To mitigate the risk associated with exposure to hypoxic environments, the SpO2 range in this study was set between 80 % and 100 %. Participant sessions with incomplete data collection or unmet hypoxic conditions were excluded from the analysis. Leave-one-out cross validation was employed to maximize the use of the limited dataset and obtain an unbiased estimate of the model’s performance (Stone, 1974). The accuracy of the smart ring’s SpO2 estimates was evaluated using the root mean square error (RMSE) between the smart ring’s measurements and those from the clinical-grade pulse oximeter, using the following equation:
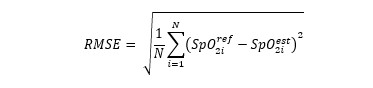
where i denotes each observation, N is the total number of data points, SpO2ref is the SpO2 value measured by the clinical-grade pulse oximeter, and SpO2est is the corresponding SpO2 estimated by the smart ring.
To apply leave-one-out cross-validation, data from one participant are withheld for validation while the SpO2 calibration is performed with the remaining participants’ data. This process is repeated for each participant to ensure subject-independent evaluation.
3. Results
The mean value of SpO2 was 88.3 ± 7.2% for the smart ring and 88.3 ± 8.0% for the clinical-grade pulse oximeter, respectively, with no significant difference observed between the two devices. Figure 3 shows the relationship between the R-values and SpO2 obtained from the clinical-grade pulse oximeter and the smart ring. The SpO2 obtained from the smart ring had an RMSE of 3.55% compared to the SpO2 measured by the medical-grade pulse oximeter.
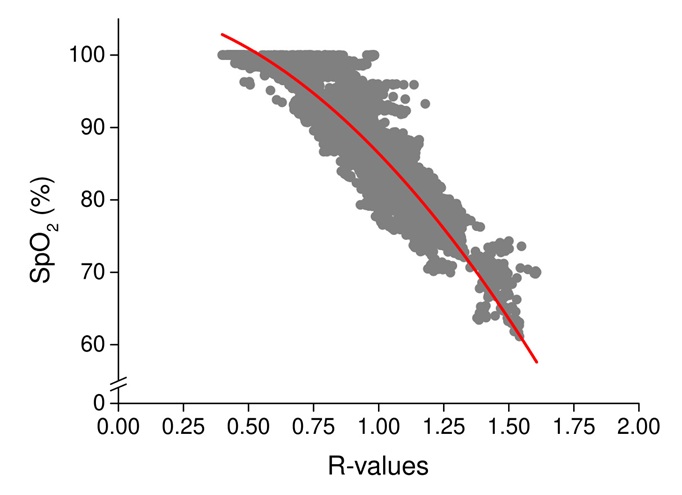
Figure 3 illustrates the relationship between SpO2 measured by a medical-grade pulse oximeter and the R-values calculated from the SOXAI smart ring, which are derived from the ratio of the AC and DC components of red and infrared light signals.
Gray dots represent 1-second synchronized measurements of SpO2 and R-values. The red line indicates the regression line derived from the relationship between SpO2 measured by the pulse oximeter and the R-values from the smart ring.
4. Discussion
The findings of this study (RMSE = 3.55%) indicate that the smart ring does not meet the stricter standard specified by the Food and Drug Administration (FDA) (RMSE < 3.5%), but sufficiently meets the standard specified in ISO 80601-2-61 (RMSE < 4.0%) (Stell et al., 2022), demonstrating adequate accuracy for a consumer-grade wearable. The RMSE of SpO2 reported in previous studies on smart rings was 2.1% (Mastrototaro et al., 2024) and 4.46% (Pracht, 2022). This level of accuracy highlights the potential of the smart ring as an accessible and user-friendly device for routine monitoring of SpO2, particularly appealing to health-conscious individuals seeking a convenient and effective tool for tracking physiological well-being.
The measurement error of SpO2 in this study (3.55%) was higher than that reported in Mastrototaro et al. (2.1%), in which participants were exposed to hypoxia environments by wearing masks and adjusting the oxygen concentration they inhaled to regulate their SpO2 levels. The analysis was performed after controlling for a stable SpO2 plateau (<2–3%) lasting more than 60 seconds. In the current study, participants were placed in a room simulating a hypoxic environment, which caused a decrease in SpO2, preventing the establishment of a stable SpO2 level as observed in the previous study (Fig. 2). Another factor that may have influenced the results is the difference in the participants’ skin color and age. Namely, variations in melanin levels in the skin play a role in light absorption and scattering, which in turn affect the SpO2 values obtained by PPG (ANALOG DEVICES, 2019). According to FDA guidelines, at least 30% of participants in studies evaluating SpO2 measurement devices should have darker skin pigmentation to ensure accuracy and fairness across diverse populations (ANALOG DEVICES, 2019). The participants in this study were exclusively Asian, whereas the previous study included four black participants out of a total of 12. Moreover, aging induces physiological changes such as pigment accumulation or depigmentation and decreases skin hydration, which alter the skin’s optical absorption and scattering properties (Kang et al., 2021). These alterations may affect the accuracy of PPG-based SpO2 measurements. The participants in the present study were relatively young (mean age: 23.3 ± 4.1 years), and the absence of age-related changes in their skin characteristics may have contributed to the relatively low RMSE observed across individuals. Collectively, differences in experimental conditions, skin pigmentation, and participant age may explain the discrepancy in measurement error between the current and previous study.
There are limitations that should be noted. First, all participants were of Asian descent, which limits the generalizability of the findings to individuals with darker skin pigmentation, as skin tone can affect the accuracy of PPG-based SpO2 measurements (Cabanas et al., 2022; Shi et al., 2022; Singh et al., 2024). Second, age-related changes in skin pigmentation, such as melanin depigmentation and redistribution, may affect the absorption and scattering of light, and thus sensor accuracy (Kang et al., 2021). Therefore, further validation is needed in populations with a broader range of skin tones and in older adults.
5. Conclusions
In conclusion, although the smart ring which incorporates novel optical elements does not yet achieve clinical-grade accuracy, it shows promising performance for a consumer-grade device. Addressing the limitations related to demographic representation and contextual variability will be essential for its development into a versatile and reliable tool for personalized health monitoring.
Author Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by HM and NO. Data analysis was conducted by SC and JW. TW and YT participated in the study design and coordinated research activities. The first draft of the manuscript was written by HM, and NO. SC, JW, and YT provided comments on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of the National Institute of Fitness and Sports in Kanoya (protocol code [https://www.nifs-k.ac.jp/research-and-collaboration/research/optout/]).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data is not publicly available due to institutional restrictions.
Acknowledgments
The authors wish to express their gratitude to the students at the National Institute of Fitness and Sports in Kanoya for their contributions to this study.
Conflicts of Interest
The authors declare no conflict of interest. SOXAI Inc, a full-time or part-time employer of several authors, supported the study by providing salary to the authors, measurement equipment, and associated firmware, but had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
ANALOG DEVICES (2019). Guidelines for SpO2 Measurement. https://www.analog.com/en/resources/technical-articles/guidelines-for-spo2-measurement–maxim-integrated.html
Cabanas, A. M., et al. (2022). Skin pigmentation influence on pulse oximetry accuracy: a systematic review and bibliometric analysis. Sensors, 22(9), 3402.
Hénault, F., et al. (2013). Design of light concentrators for Cherenkov telescope observatories. In Nonimaging Optics: Efficient Design for Illumination and Solar Concentration X (Vol. 8834, pp. 13-24). SPIE.
Kang, H.Y., et al. (2021). Alterations of the pigmentation system in the aging process. Pigment Cell Melanoma Res, 34:800-813.
Lu, C.H., et al. (2015). Design of a ring-type reflection pulse oximeter with a parabolic reflector. Biomedical Engineering: Applications, Basis and Communications, 27 (01),1550007.
Mastrototaro, J. J., et al. (2024). Performance of a Wearable Ring in Controlled Hypoxia: A Prospective Observational Study. JMIR Formative Research, 8, e54256.
Otani, N., et al. (2023). Creating an in vivo hypoxic environment by gas inhalation for the potential evaluation of new pulse oximeters. Translational and Regulatory Sciences, 5(1), 23-27.
Pracht, M. (2022). Optimized blood oxygen saturation level measurements using a novel constellation of PPG modules from a Smart Ring (master’s thesis). University of Bern.
Shi, C., et al. (2022). The accuracy of pulse oximetry in measuring oxygen saturation by levels of skin pigmentation: a systematic review and meta-analysis. BMC medicine, 20(1), 267.
Singhal, A., et al. (2023). Arterial oxygen saturation: A vital sign?. Nigerian journal of clinical practice, 26(11), 1591-1594.
Singh, S., et al. (2024). Impact of skin pigmentation on pulse oximetry blood oxygenation and wearable pulse rate accuracy: Systematic review and meta-analysis. Journal of Medical Internet Research, 26, e62769.
Stell, D., et al. (2022). Exploring the impact of pulse oximeter selection within the COVID-19 home-use pulse oximetry pathways. BMJ Open Respiratory Research, 9(1).
Stone, M. (1974). Cross-validatory choice and assessment of statistical predictions. Journal of the Royal Statistical Society: Series B (Methodological), 36(2), 111–147.
Relevant Articles
-

Impact of Three-Dimensional Multiple Object Tracking (3D-MOT) on Cognitive Performance and Brain Activity in Soccer Players
by Yoshiko Saito - 2025,S9
VIEW -

Pilot study on changes in frontal oxygenated hemoglobin levels in beginners during practice of Karate Forms
by Kiyohisa Natsume - 2026,3
VIEW -

Why do you recall that smelly food? Effects of childhood residence region and potential reinforcing effect of marriage
by Yoshinori Miyamura - 2026,2
VIEW -

A Study on the Effectiveness of Glycerophosphocholine (α-GPC) as an e-Sports Supplement
by Yuki Kamioka - 2025,5
VIEW



