Search for Articles
Article Electrical and Electronic Engineering Interdisciplinary Sciences
Real-Time Physiological Monitoring for Management of Normobaric Hypoxic Training Toward Wearable System Implementation
Journal Of Digital Life.2022, 2,2;
Received:January 25, 2022 Revised:February 8, 2022 Accepted:February 17, 2022 Published:February 28, 2022
- Kazuki Hisatsune
- Department of Computer Science and Electrical Engineering, Graduate School of Science and Technology, Kumamoto University
- Toshitaka Yamakawa
- Division of Informatics and Energy, Faculty of Advanced Science and Technology, Kumamoto University
Correspondence: yamakawa@cs.kumamoto-u.ac.jp
Abstract
As a method to prevent lifestyle diseases, normobaric hypoxic training has been attracting attention. However, its exercise load and safety in non-athletes remain unclear. In this study, 20 healthy university students underwent a 15-min exercise test in a normobaric hypoxic room set at two different oxygen concentrations (O2: 20% and 16%), and the exercise load and safety were evaluated. The test comprised walking within the upper and lower limits of the heart rate (HR) calculated via the Karvonen method. The results showed that in case of 16% O2, the same energy was consumed despite significantly lower walking speed and distance than those in case of 20% O2. Therefore, it is suggested that the Karvonen method is effective in setting the load for hypoxic training. In addition, real-time monitoring of arterial oxygen saturation (SpO2) could be used to evaluate the safety of hypoxic training. Based on these results, we have developed a wearable pulse oximeter that can measure both HR and SpO2 from the earlobe and a dedicated smartphone application for analysis. If these can be practically applied, hypoxic training can be conducted safely that will contribute to the prevention of lifestyle diseases and the consequent extension of healthy life expectancy.
1. Introduction
In 2018, the World Health Organization estimated that 71% of all deaths worldwide are attributed to lifestyle diseases (World Health Organization, 2018). Lifestyle diseases are a general term for diseases caused by lifestyle and are a major cause of serious diseases. Diet and exercise therapies are recommended for the prevention of lifestyle diseases (Budreviciute et al., 2020) and for improvement of lifestyle. Currently, hypoxic training, wherein exercise is performed in a hypoxic environment, is gaining attention as an effective method of exercise therapy (Lizamore & Hamlin., 2017; Millet et al., 2016). When an exercise is performed in a hypoxic environment, the oxygen-carrying capacity of the muscles is improved by increasing the hemoglobin concentration and the number of red blood cells (Hauser et al., 2016). Additionally, exercise in a hypoxic environment is considered to be an effective therapy for people with low physical fitness and obesity because it may possibly have sufficient effects even with a low exercise load in comparison with exercise in a normal oxygen environment (Fernández Menéndez et al., 2018; Katayama et al., 2010).
Traditionally, hypoxic environments have been used for high altitude training in the field of competitive sports. Live-high/train-high involving going to high altitudes to train, is often used, and training is often conducted in a hypobaric hypoxic environment. However, training in hypobaric hypoxic environments leads to typical altitude sickness symptoms such as headache and dizziness. As a result, athletes cannot train routinely owing to the physical conditions. Therefore, live-high/train-low, wherein people live at high altitudes and train at low altitudes, is now the mainstream (Saugy et al., 2014). However, since most of the time is spent in a hypoxic environment, it is difficult for everyone, except competitive athletes, to safely benefit from the hypoxic environment. Therefore, a method of training in a normobaric hypoxic room at a normal altitude is gaining attention. Under normal pressure, the risks of headache and dizziness are lower than those at high altitudes (Saugy et al., 2014). In addition, a hypoxic room allows users to set the oxygen concentration based on their individual needs, making it safer than training at high altitudes. However, the response of non-athletes to the hypoxic load is estimated to vary widely among individuals, unlike competitive athletes who routinely undergo cardiopulmonary load exercise. Even though Adequate knowledge of exercise intensity and safety in non-athletes would provide a variety of benefits for hypoxic training, the physiological measures to assess the exercise load and safety of hypoxic training in non-athletes is still unclear (Millet et al., 2016; Mourot L., 2018).
In previous studies, the heart rate (HR) criterion has been used to assess the exercise load of hypoxic training (Gutwenger et al., 2015; Park & Lim., 2017). It has also been reported that the various positive effects of hypoxic training may be caused by the decrease in SpO2 during such training (Dinenno., 2016; Joyner & Casey., 2014; Manimmanakorn et al., 2013) even though a serious SpO2 decrease leads hypoxemia. From these findings, simultaneous measurement of HR and SpO2 during hypoxic training may contribute to evaluating exercise load and safety in non-athletes. In addition, development of a wearable monitoring system that measures HR and SpO2 and evaluates the load with real-time calculation enables automated management of safe and efficient hypoxic training.
In this study, a 15-min exercise test was conducted on a self-propelled treadmill in a normobaric hypoxic room set at two different oxygen concentrations (O2: 20% as a normoxia control, 16% as a hypoxic condition equivalent to 2,000 m altitude) in order to develop a wearable monitoring system with easy operation to evaluate exercise load and safety during normobaric hypoxic training. Based on the Karvonen method, we tested whether it is effective to control the exercise load in 20 subjects by setting the upper and lower limits of HR. We also examined whether the safety of hypoxic training could be evaluated based on SpO2. The potential for implementation into a wearable system of automated training management using real-time analysis of HR and SpO2 is shown with a prototype design.
2. Materials and Methods
2.1 Experimental procedure
Twenty healthy university students with no cardiovascular and respiratory diseases were selected as the experimental subjects. In selecting the subjects, a checklist was used to confirm that there was no history of cardiovascular and respiratory disease. Informed consent for participation in the study was obtained from all the participants.
The exercise test was performed on a self-propelled treadmill (Matrix S-Drive, Johnson Health Tech, Tokyo, Japan) with an inclination angle of 7° in a hypoxic room set at two different oxygen concentrations (20% and 16%) using a hypoxia generator (YHS-C10, Hypotec, Tokyo, Japan). The exercise load was controlled based on the target heart rate (HRtgt) calculated using the Karvonen method (Karvonen & Voutilainen., 1988; Young-McCaughan & Arzola., 2007). First, to calculate HRtgt, the maximum heart rate (HRmax) was calculated using Formula (1) (She et al., 2015). In Formula (1), age is the age of the subject. Next, the heart rate reserve (HRR) was calculated using Formula (2) (Kurl et al., 2021). In Formula (2), HRrest is the resting heart rate. Finally, HRtgt was calculated using Formula (3). EI in Formula (3) represents the exercise intensity. The American College of Sports Medicine recommends an EI range of 40%–85% for healthy individuals (American College of Sports Medicine, 2012). Furthermore, a previous study demonstrated that obese individuals start with an EI in the range 40−60% and gradually increase their EI; in addition, to increase the maximal oxygen uptake, EI should be increased to 50−70% (Saris et al., 2003). In the present experiment, based on these recommendations approved by two experienced trainers, the lower and upper limits of HRtgt were calculated by setting EI to 60% and 75%.
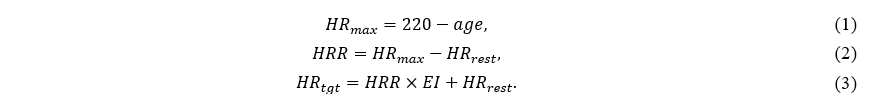
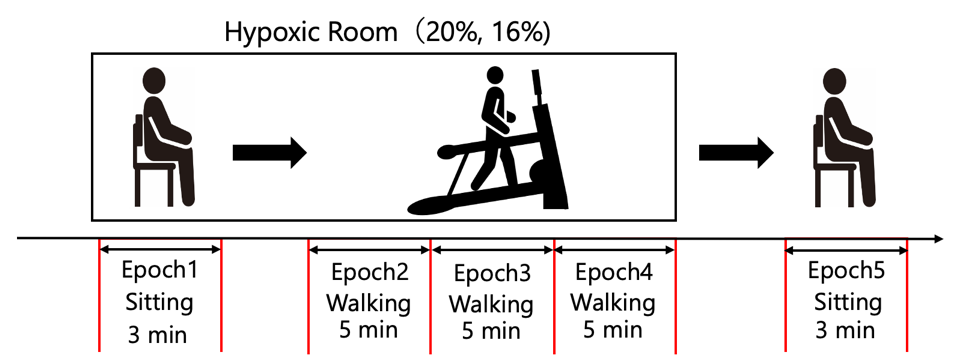
First, the subjects were requested to sit for 3 min in a hypoxic room set at an appropriate oxygen concentration to determine whether they could perform the exercise test. Next, using LabChart Pro (ver. 8.1.17, ADInstruments, Dunedin, New Zealand), the average of the HR acquired during the last 1 min before the termination of the resting in sitting position, was calculated and used as HRrest. Formula (1–3) were subsequently used to calculate the upper and lower limits of HRtgt. Thereafter, using a self-propelled treadmill, the subjects walked for 15 min within the upper and lower limits of the HRtgt. Finally, the subjects were requested to sit for 3 min outside the hypoxic room, and if there were no problems with their physical condition, the procedure was completed. The protocol and the epochs definition are illustrated in Fig.1.
The exercise tests at each oxygen concentration were conducted on the same day. Ten of the 20 subjects performed the exercise test under the condition of 16% O2 after the performance of the exercise test under the condition of 20% O2. The remaining 10 subjects performed the exercise test under the condition of 20% O2 after the performance of the exercise test under the condition of 16% O2. The exercise test was stopped when any of the following discontinuance criteria were met:
- If the time exceeding the upper limit of HRtgt was more than 1 min and the experimenter decides to discontinue the exercise load.;
- If the SpO2 displayed on the oxygen saturation monitor was less than 85% for more than 1 min and the experimenter decides to discontinue the exercise load.;
- When the experimenter ascertained the considerable difficulty in continuance of the exercise load.
Electrocardiograms (ECG) were measured from typical lead II using an electrocardiogram (BSM-3400, Nihon Kohden, Tokyo, Japan). SpO2 was measured from the subject’s right earlobe using an ear clip sensor (MLT332, ADInstruments, Otago, New Zealand). The pulse signal corresponding to the rotation speed of the treadmill was measured using a length counter (CT1-3:10A, Line Seiki, Tokyo, Japan). Energy expenditure (EE) during walking was measured using a research activity meter (HJA-750C, Omron Healthcare, Kyoto, Japan) attached to the waist of the subject. ECG, SpO2, and pulse signals were collected using an eight-channel biological amplifier (PL3508, ADInstruments, Otago, New Zealand) and recorded using LabChart Pro. HR was continuously calculated from the R-wave intervals of the ECG using LabChart Pro. The walking velocity was continuously calculated from the pulse signal using LabChart Pro. ECG, HR, SpO2, and velocity were recorded in real-time during the entire exercise test. EE was recorded after the completion of the experiment using a dedicated software (ver. 2.2, Omron Healthcare, Kyoto, Japan). The walking distance was recorded as the value displayed on the monitor attached to the treadmill. The percentage of time that the lower limit of the HRtgt exceeded during the 15-min walk was calculated as the exercise achievement rate (AR).
The study was conducted in accordance with the guidelines of the Declaration of Helsinki and approved by the Ethics Review Committee of the School of Advanced Science and Technology, Kumamoto University (protocol code R3-4).
2.2 Data Analysis
The measured HR and SpO2 values contained outliers due to false detection of R-waves by LabChart Pro, motion artifacts during walking, and poor contact between the earlobe and ear clip. Therefore, referring to a previous study (Hampel., 1974; Pearson et al., 2015), outliers in HR and SpO2 were detected using a 30-s moving window. An outlier was defined as an element that was away from more than three times the median absolute deviation (MAD) of the data x within a 30-s moving window. The MAD was calculated using Formula (4). The detected outliers were replaced by previous non-outliers.

In reference to a previous study (Horiuchi et al., 2019), we calculated HR, SpO2, and velocity as the mean value of the measured data 1 min before the end of each Epoch. Furthermore, we calculated EE, distance, and AR as the mean values of the 15 min data obtained after the exercise test.
Based on previous studies (Ikeda, 2013a, b), we conducted comparison between the two groups using the Wilcoxon signed-rank test, each group comprising data measured at 20% and 16% O2. Furthermore, referring to published guidelines (Mizumoto & Takeuchi, 2008), we calculated the effect size (r) after the Wilcoxon signed-rank test. The values of Epoch1 and Epoch4 were used for HR. SpO2 and velocity were collected from Epoch4. The significance level was set at 0.01.
3. Results
None of the subjects met the criteria for discontinuation of the experiment. Therefore, 20 subjects were included in the analysis (Age: 22.0±1.0 years, Height: 170±5.6 cm, Weight: 60.8±8.1 kg, Body mass index: 21.0±2.4 kg/m2).
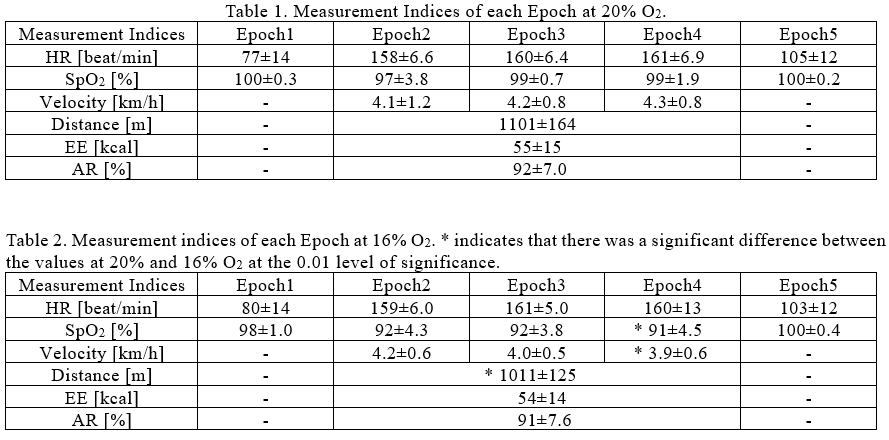
The HR, SpO2, velocity, EE, distance, and AR are summarized for each epoch, as shown in Tables 1 and 2. The values in the table are the mean ± standard deviation. In this experiment, no subject exceeded the upper limit of the HRtgt for more than 1 min. In addition, the lowest SpO2 value during exercise was approximately 84%; however, it did not continue for more than 1 min and did not satisfy the discontinuation criteria.
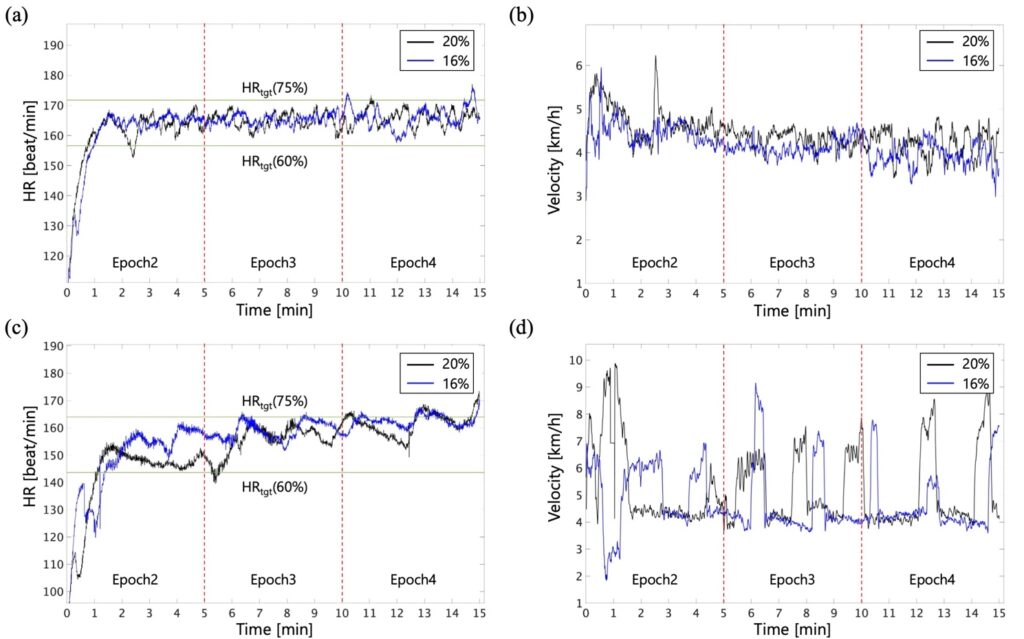
Time series plots of HR and velocity during walking of subjects 3 and 9 are shown in Fig.2. The plot for subject 3 shows typical response in HR and velocity. The plot for subject 9 shows noticeable difference between the HR and velocity from the other subjects. Figs.2(a) and (c) show that both subjects walked within the upper and lower limits of the HRtgt. Fig.2(b) shows that the velocity of subject 3 was in the range of approximately 4–5 km/h, except at the beginning of walking. Furthermore, Fig.2(d) shows that the velocity of subject 9 changed significantly throughout, except at the beginning of walking.
The results of the Wilcoxon signed-rank test showed that the HR values were not significantly different between the 20% and 16% O2 in both Epoch 1 and Epoch 4 (Epoch 1: p = 0.10, r = 0.37, Epoch 4: p = 0.35, r = 0.21). The results also showed that SpO2 values at 16% O2 were significantly lower than those at 20% O2 (p = 0.0019, r = 0.83). The values of the velocity and distance at 16% oxygen concentration were significantly lower than those at 20% O2 (velocity: p = 0.0012, r = 0.73, distance: p = 0.00020, r = 0.83). The values of EE and AR were not significantly different between 20% and 16% O2 (EE: p = 0.35, r = 0.20, AR: p = 0.25, r = 0.26).
4. Discussion
Tables 1 and 2 show that there was no significant difference between HR and AR during exercise and the values were almost the same. However, the values of the velocity and distance at 16% O2 were significantly lower than those in the 20% O2. The EE values are almost the same with no significant difference between 20% and 16% O2. Therefore, exercise under 16% O2 can be expected to provide the same energy expenditure with a significantly lower velocity and distance relative to 20% O2. These results support previous studies that show that exercise therapy in a normobaric hypoxic environment is effective for obese, diabetic, and elderly people with low physical fitness (Fernández Menéndez et al., 2018; Haufe et al., 2008; Lizamore & Hamlin., 2017; Pramsohler et al., 2017; Wiesner et al., 2010).
As shown in Figs.2(a) and (b), subjects whose HR value did not decrease significantly after exceeding the lower limit of HRtgt once exhibited almost no change in velocity. In contrast, subjects whose HR value was recovered during exercise, regardless of the oxygen concentration, exhibited an increase in velocity at approximately 5 min and 30 s, as shown in Figs.2(c) and (d), respectively. Furthermore, the HR value was controlled when it exceeded the upper limit of HRtgt, similar to that at 10 min and 20 s, by lowering the velocity. The HR value of other subjects was maintained within the upper and lower limits of HRtgt by adjusting their velocities. Monitoring the HR value of athletes and patients undergoing exercise therapy is very common and practically useful (Achten & Jeukendrup., 2003; Casillas et al., 2017). In this experiment, we used the Karvonen method to set the upper and lower limits of HRtgt, based on which subjects could easily judge the overload or underload of exercise by themselves and control their walking. Results suggested that the real-time monitoring of HR using the Karvonen method helped obtain a sufficient EE under adequate cardiac load even in a hypoxic environment.
Table 2 shows that the mean value of SpO2 during exercise under the normoxic condition decreased by only approximately 3% from the mean value in Epoch1. The mean value under 16% O2 during exercise decreased by approximately 7% compared with Epoch1. Furthermore, the SpO2 values of Epoch4 in 16% O2 were significantly lower than those in 20% O2. This result is similar to that of a previous study in which exercise tests were performed in 20% and 15% O2 (Morishima et al., 2014). It has been reported that a decrease in SpO2 due to the effects of hypoxic environment contributes to vasodilation, which facilitates the supply of blood and oxygen to muscles (Dinenno., 2016; Joyner & Casey., 2014). Results indicated that SpO2 reflected the hypoxic load and could be used as an index to evaluate the effect of hypoxic training.
In this experiment, the minimum SpO2 was about 84%. However, it had recovered to 85% or higher without continuing for more than 1 min. Therefore, the discontinuation criteria for the experiment were not met. In addition, no cases of acute mountain sickness or respiratory failure were reported, and no adverse events requiring medical treatment were observed. A steep drop in SpO2 can lead to acute mountain sickness and poor physical condition (Saugy et al., 2014). These results suggest that maintaining a SpO2 of 85% or higher employing real-time monitoring is useful as a safety criterion for hypoxic training in non-athletes.
One of the limitations of this study is that we compared only the acute effects of different oxygen concentrations during exercise. It is desired to verify the effects of long-term exercise with analyzing improvement of body composition indices in a future work.
5. Development of a Wearable Real-time Monitoring System
This study suggests that hypoxic training can be conducted with assessing HR and SpO2 to manage load and safety. Toward implementation into a small and user-friendly monitoring system, we developed a wearable pulse oximeter that can measure both HR and SpO2 from the earlobes using transmission-type photoplethysmography, as shown in Figs.3(a) and (b). A dedicated smartphone application (Fig.3(c)) was designed to achieve automated training management employing real-time HR and SpO2 analysis.
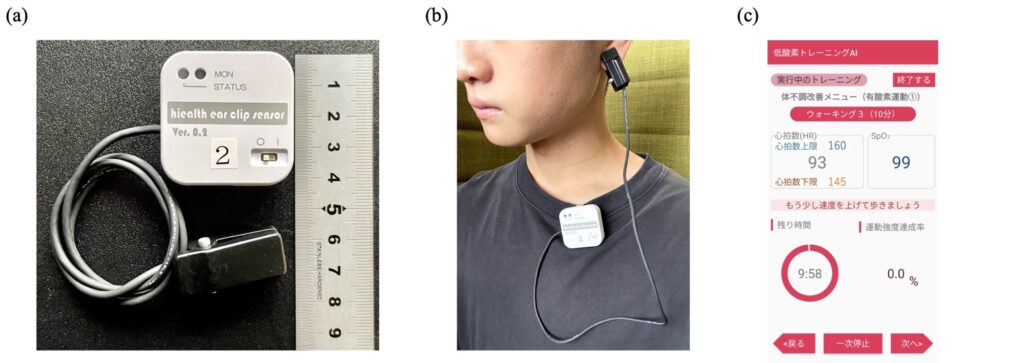
The dimensions of the main body of the transmitter shown as the white rounded square case in Fig.3(a) are 38 mm × 38 mm × 13 mm. The total weight of the entire device is less than 30 g. We achieved such miniaturization and weight reduction by leveraging flexible printed circuit technology to develop a frontend circuit for the ear clip (implemented in the black ear-clip case) and two circuit boards stacked vertically in the main body to realize signal processing and transmitter functions within a small and light form factor achieving good wearability in exercise activity. In addition, the use of measurements from the earlobes improves the motion artifact tolerance relative to measurements from the fingertips especially during exercise. It also has a clasp on the back of the main body to clip on the user’s clothing, as shown in Fig.3(b).
The developed device is equipped with a Bluetooth module that transmits the measured HR and SpO2 data to a smartphone for monitoring and recording.
The dedicated smartphone application has several exercise programs with different ranges of EI, allowing users to select the program that best suits their purpose. During the exercise program, the screen shown in Fig.3(c) is displayed. This screen displays the upper and lower limits of HRtgt, current HR, SpO2, time remaining for exercise, and AR. If the HR is below the lower limit of HRtgt, an instruction to increase velocity is displayed. Conversely, if the HR is above the upper limit of HRtgt, an instruction to lower velocity is displayed. In addition, if the SpO2 is below 85% for more than 1 min, instructions to stop exercising and take a rest immediately will be displayed. In this manner, the dedicated smartphone application enables a user to exercise safely.
Accuracy verification under the operation test combining the device and application is remained to be accomplished in future works. The monitoring system with the developed device and app can improve the safety of hypoxic training and reduce operational costs, thereby ensuring that hypoxic training becomes more prevalent.
6. Conclusions
In this study, 20 healthy subjects underwent an exercise test by walking for 15 min within the upper and lower limits of HRtgt calculated using the Karvonen method in a hypoxic room set at 20% and 16% O2. The results showed that exercise under the environmental condition of 16% O2 had significantly lower velocity and distance compared with those under the condition of 20% O2, even though HR and EE were almost equal. Therefore, it was suggested that real-time monitoring of HR and the Karvonen method contribute in obtaining a sufficient EE under the adequate cardiac load even in the hypoxic environments. These results based on the Karvonen method suggest that hypoxic training is effective for obese and elderly people with low exercise tolerance. In addition, SpO2 reflected the hypoxic load and could be used as an index to evaluate the effectiveness and safety of hypoxic training. These results showed that real-time monitoring of HR and SpO2 can be used to evaluate the exercise load and safety of hypoxic training. Furthermore, the practical application of the device developed that can measure HR and SpO2 from the earlobe and the dedicated application is expected to improve the safety of hypoxic training and lower the operational cost. This is expected to contribute to the widespread use of hypoxic training, thereby contributing to the prevention of lifestyle diseases and the extension of healthy life expectancy.
Author Contributions
Conceptualization: K.H. and T.Y.; methodology: K.H. and T.Y.; software: K.H. and T.Y.; validation: K.H. and T.Y.; formal analysis: K.H. and T.Y.; investigation: K.H. and T.Y.; resources: K.H. and T.Y.; data curation: K.H.; writing—original draft preparation: K.H.; writing—review and editing: K.H. and T.Y.; visualization: K.H. and T.Y.; supervision: T.Y.; project administration: K.H. and T.Y.; All authors have read and agreed to the published version of the manuscript.
Funding
This research was partially supported by the New Collaboration flamework of the Small and Medium Enterprise Agency of Japan (Grant number R2-37).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the School of Advanced Science and Technology, Kumamoto University (protocol code R3-4 and date of approval September 6, 2021).
Informed Consent Statement
Written informed consent was obtained from all subjects involved in the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
Achten, J., & Jeukendrup, A. E. (2003). Heart rate monitoring: applications and limitations. Sports medicine (Auckland, N.Z.), 33(7), 517–538. https://doi.org/10.2165/00007256-200333070-00004
American College of Sports Medicine. (2012). ACSM’s resource manual for guidelines for exercise testing and prescription. Lippincott Williams & Wilkins.
Budreviciute, A., Damiati, S., Sabir, D. K., Onder, K., Schuller-Goetzburg, P., Plakys, G., Katileviciute, A., Khoja, S., & Kodzius, R. (2020). Management and Prevention Strategies for Non-communicable Diseases (NCDs) and Their Risk Factors. Frontiers in public health, 8, 574111. https://doi.org/10.3389/fpubh.2020.574111
Casillas, J. M., Gudjoncik, A., Gremeaux, V., Aulagne, J., Besson, D., & Laroche, D. (2017). Assessment tools for personalizing training intensity during cardiac rehabilitation: Literature review and practical proposals. Annals of physical and rehabilitation medicine, 60(1), 43–49.
Dinenno, F. A. (2016). Skeletal muscle vasodilation during systemic hypoxia in humans. Journal of Applied Physiology, 120(2), 216–225. https://doi.org/10.1152/japplphysiol.00256.2015
Fernández Menéndez, A., Saudan, G., Sperisen, L., Hans, D., Saubade, M., Millet, G. P., & Malatesta, D. (2018). Effects of short-term normobaric hypoxic walking training on energetics and mechanics of gait in adults with obesity. Obesity, 26(5), 819–827. https://doi.org/10.1002/oby.22131
Gutwenger, I., Hofer, G., Gutwenger, A. K., Sandri, M., & Wiedermann, C. J. (2015). Pilot study on the effects of a 2-week hiking vacation at moderate versus low altitude on plasma parameters of carbohydrate and lipid metabolism in patients with metabolic syndrome. BMC research notes, 8, 103. https://doi.org/10.1186/s13104-015-1066-3
Hampel, F. R. (1974). The influence curve and its role in robust estimation. Journal of the American Statistical Association, 69(346), 383–393. https://doi.org/10.2307/2285666
Haufe, S., Wiesner, S., Engeli, S., Luft, F. C., & Jordan, J. (2008). Influences of normobaric hypoxia training on metabolic risk markers in human subjects. Medicine & Science in Sports & Exercise, 40(11), 1939–1944. https://doi.org/10.1249/MSS.0b013e31817f1988
Hauser, A., Schmitt, L., Troesch, S., Saugy, J. J., Cejuela-Anta, R., Faiss, R., Robinson, N., Wehrlin, J. P., & Millet, G. P. (2016). Similar Hemoglobin Mass Response in Hypobaric and Normobaric Hypoxia in Athletes. Medicine & Science in Sports & Exercise, 48(4), 734–741. https://doi.org/10.1249/MSS.0000000000000808
Horiuchi, M., Kirihara, Y., Fukuoka, Y., & Pontzer, H. (2019). Sex differences in respiratory and circulatory cost during hypoxic walking: potential impact on oxygen saturation. Scientific Reports, 9(1), 1–10. https://doi.org/10.1038/s41598-019-44844-6
Ikeda, I, (2013a). [For those who use statistical tests without understanding them II] (in Japanese). Kagaku to Seibutsu, 51(6), 408–413. https://doi.org/10.1271/kagakutoseibutsu.57.562
Ikeda, I, (2013b). [For those who use statistical tests without understanding them III] (in Japanese). Kagaku to Seibutsu, 51(7), 483–495. https://doi.org/10.1271/kagakutoseibutsu.51.483
Joyner, M. J., & Casey, D. P. (2014). Muscle blood flow, hypoxia, and hypoperfusion. Journal of Applied Physiology, 116(7), 852–857. https://doi.org/10.1152/japplphysiol.00620.2013
Karvonen, J., & Vuorimaa, T. (1988). Heart rate and exercise intensity during sports activities. Practical application. Sports Medicine, 5(5), 303–311. https://doi.org/10.2165/00007256-198805050-00002
Katayama, K., Goto, K., Ishida, K., & Ogita, F. (2010). Substrate utilization during exercise and recovery at moderate altitude. Metabolism: Clinical and experimental, 59(7), 959–966. https://doi.org/10.1016/j.metabol.2009.10.017
Kurl, S., Jae, S. Y., Voutilainen, A., Hagnäs, M., & Laukkanen, J. A. (2021). Exercise heart rate reserve and recovery as risk factors for sudden cardiac death. Progress in Cardiovascular Diseases, 68, 7–11. https://doi.org/10.1016/j.pcad.2021.09.002
Lizamore, C. A., & Hamlin, M. J. (2017). The use of simulated altitude techniques for beneficial cardiovascular health outcomes in nonathletic, sedentary, and clinical populations: A literature review. High Altitude Medicine & Biology, 18(4), 305–321. https://doi.org/10.1089/ham.2017.0050
Manimmanakorn, A., Manimmanakorn, N., Taylor, R., Draper, N., Billaut, F., Shearman, J. P., & Hamlin, M. J. (2013). Effects of resistance training combined with vascular occlusion or hypoxia on neuromuscular function in athletes. European journal of applied physiology, 113(7), 1767–1774. https://doi.org/10.1007/s00421-013-2605-z
Millet G. P., Debevec T., Brocherie F., Malatesta D., & Gigard O. (2016). Therapeutic use of exercising in hypoxia: promises and limitations. Frontiers in Physiology, 7(224). https://doi.org/10.3389/fphys.2016.00224.
Mizumoto, A., & Takeuchi, O. (2008). [Basics and Considerations for Reporting Effect Sizes in Research Papers] (in Japanese). A bulletin for the teachers of English, 31, 57–66.
Morishima, T., Mori, A., Sasaki, H., & Goto, K. (2014). Impact of exercise and moderate hypoxia on glycemic regulation and substrate oxidation pattern. PLOS One, 9(10), e108629. https://doi.org/10.1371/journal.pone.0108629
Mourot L. (2018). Limitation of Maximal Heart Rate in Hypoxia: Mechanisms and Clinical Importance. Frontiers in physiology, 9, 972. https://doi.org/10.3389/fphys.2018.00972
Nakai, k., Watanabe, H., Takahashi, S., Miyamoto, H., Doi, A., Hanakuma, A., Morishita, Y., Sawada, T., Otsuji, M., Hirate, Shindo. Y., & Kosuge, K. (2009). A new approach of the percutaneous arterial oxygen saturation (SpO2) measurement – challenge of earlobe probe sensor (in Japanese). Medical Device Science, 79(8), 638–646. https://doi.org/10.4286/jjmi.79.638
Park H.-Y., Lim K. (2017). The effects of aerobic exercise at hypoxic condition during 6 weeks on body composition, blood pressure, arterial stiffness, and blood lipid level in obese women. Int. J. Sports Sci. Med., 1, 1–5
Pearson, R. K., Neuvo, Y., Astola, J., & Gabbouj, M. (2015). The class of generalized hampel filters. In 2015 23rd European Signal Processing Conference (EUSIPCO) (pp. 2501–2505), IEEE. https://doi.org/10.1109/EUSIPCO.2015.7362835
Pramsohler, S., Burtscher, M., Faulhaber, M., Gatterer, H., Rausch, L., Eliasson, A., & Netzer, N. C. (2017). Endurance training in normobaric hypoxia imposes less physical stress for geriatric rehabilitation. Frontiers in Physiology, 8, 514. https://doi.org/10.3389/fphys.2017.00514
Saris, W. H., Blair, S. N., van Baak, M. A., Eaton, S. B., Davies, P. S., Di Pietro, L., Fogelholm, M., Rissanen, A., Schoeller, D., Swinburn, B., Tremblay, A., Westerterp, K. R., & Wyatt, H. (2003). How much physical activity is enough to prevent unhealthy weight gain? Outcome of the IASO 1st Stock Conference and consensus statement. Obesity Reviews, 4(2), 101–114. https://doi.org/10.1046/j.1467-789x.2003.00101
Saugy, J. J., Schmitt, L., Cejuela, R., Faiss, R., Hauser, A., Wehrlin, J. P., Rudaz, B., Delessert, A., Robinson, N., & Millet, G. P. (2014). Comparison of “Live High-Train Low” in normobaric versus hypobaric hypoxia. PLoS One, 9(12), e114418. https://doi.org/10.1371/journal.pone.0114418
She, J., Nakamura, H., Makino, K., Ohyama, Y., & Hashimoto, H. (2015). Selection of suitable maximum-heart-rate formulas for use with Karvonen formula to calculate exercise intensity. International Journal of Automation and Computing, 12(1), 62–69. https://doi.org/10.1007/s11633-014-0824-3
World Health Organization. (2018). Noncommunicable diseases country profiles 2018. World Health Organization.
Wiesner, S., Haufe, S., Engeli, S., Mutschler, H., Haas, U., Luft, F. C., & Jordan, J. (2010). Influences of normobaric hypoxia training on physical fitness and metabolic risk markers in overweight to obese subjects. Obesity, 18(1), 116–120. https://doi.org/10.1038/oby.2009.193
Young-McCaughan, S., & Arzola, S. M. (2007). Exercise intervention research for patients with cancer on treatment. Seminars in Oncology Nursing, 23(4), 264–274. https://doi.org/10.1016/j.soncn.2007.08.004
Relevant Articles
-

An Inquiry-Based Learning Support System for Children in Sports Acquisition Processes
by Masayuki Yamada - 2024,3
VIEW -

Clarifying the Sharpened network diversity in French flair rugby
by Koh Sasaki - 2024,2
VIEW -

Review matching task to diagnose basic review ability
by Koki Saito - 2024,1
VIEW -

The Effects of Positive and Negative Ions on esports Performance and Arousal Levels Part 2 -Testing Higher Ion Density-
by Goichi Hagiwara - 2024,S3
VIEW



